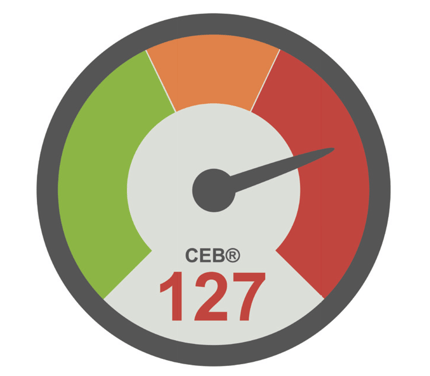
The Cardiac Electrical Biomarker (CEB®) is a calculation based on the corpuls ECGmax capability. The output from this calculation is a simple and informative alert system, showing the likelihood of myocardial ischemia almost instantaneously, with comparable sensitivity and specificity to troponin. The key features of the CEB® are;
> Simple interpretation using the traffic light concept
> Measured value is comparable to troponin
> Fast reaction by measuring the electric field
> High sensitivity and specificity
> No additional electrodes required
> Continuous value
> Non-invasive measurement
The CEB® in Detail
When a heart beats, a dipolar electrical field is created which can be measured between two electrodes attached to the body, say for example in an ECG (electrocardiogram).
When a patient suffers acute myocardial ischemia (AMI), reducing or even stopping the blood flow to the heart, the dipolar electrical field is disturbed. It is now possible to use these disturbances in the electrical field to determine myocardial injury. The resultant tool that translates these disturbances in to a marker of myocardial injury is known as the Cardiac Electrical Biomarker (CEB®).
CEB® is constructed from three ECG leads of the standard ECG electrode set and has high diagnostic accuracy by analysing ECG changes (Schreck and Fishberg 2013). The current gold standard for a specific diagnosis of myocardial injury is the highly sensitive cardiac troponin I (Hs-cTnI). Hs-cTnI is a marker for myocardial necrosis (cell death).
Typically, Hs-cTnI should be measured at clinical presentation and 3 hours after admission for 100% sensitivity and negative predictive value (Thygesen et al. 2012). A study conducted by Tereshchenko et al. (2014) explored the correlation between troponin and CEB® in 3 hour steps. They showed significant correlation between troponin and CEB® for the second and third 3 hour period after presentation of the patient. Strebel et al. (2018) stated a weak but significant correlation between troponin and CEB® also at the time of presentation. Consequently, the CEB® is instantly available the moment an ECG is measured. Rather than 3 hours, only 10 seconds are required until a CEB® result is available.
 The Cardia Electrical Biomarker
The Cardia Electrical Biomarker
The higher the CEB® number, the higher the multipolar activity and consequently the probability of acute myocardial ischemic injury. A receiver-operating-characteristic analysis showed that a value of 65 and smaller indicates a normal dipolar electrical heart, while a value of 95 and higher is a clear indication to suggest acute myocardial injury. The zone between 66 and 94 is indeterminate, but these cases occurred in only 10% of the patients (Schreck and Fishberg 2013).
Even though there were a number of indeterminate CEB®s included as false positive or false negative results, analyzing the correlation of a diagnosis with the CEB® and the diagnosis of different physicians still shows a noninferiority of the CEB®. (Schreck and Fishberg 2013). In summary, the CEB® is simultaneously available with the ECG, it shows high diagnostic accuracy, troponin I correlation and correlation to physicians’ diagnostic ECG interpretation. This technology allows immediate identification of patients with AMII on scene (Schreck and Fishberg 2013).
REFERENCES
Schreck, D. M.; Fishberg, R. D. (2013): Diagnostic Accuracy of a New Cardiac Electrical Biomarker for Detection of Electrocardiogram Changes Suggestive of Acute Myocardial Ischemic Injury. In: Annals of Non-invasive Electrocardiology 19 (2), S. 129–144. DOI: 10.1111/anec.12109.
Schreck, D. M.; Fishberg, R. D. (2015): Detection of acute myocardial ischemic injury by gender using a novel cardiac electrical biomarker. In: The American journal of emergency medicine 33 (3), S. 383–390. DOI: 10.1016/j.ajem.2014.12.029.
Strebel, I.; Twerenbold, R.; Boeddinghaus, J.; Abächerli, R.; Rubini Giménez, M.; Wildi, K. et al. (2018): Diagnostic value of the cardiac electrical biomarker, a novel ECG marker indicating myocardial injury, in patients with symptoms suggestive of non-ST-elevation myocardial infarction. In: Annals of non-invasive electrocardiology : the official journal of the International Society for Holter and Non-invasive Electrocardiology, Inc 23 (4), e12538. DOI: 10.1111/anec.12538.
Tereshchenko, L. G.; Gatz, D.; Feeny, A.; Korley, F. K. (2014): Automated analysis of the 12-lead ECG in the emergency department. Association between high-sensitivity cardiac troponin I and the cardiac electrical biomarker. In: Critical pathways in cardiology 13 (1), S. 25–28. DOI: 10.1097/ HPC.0000000000000006.
Thygesen, K.; Mair, J.; Giannitsis, E.; Mueller, C.; Lindahl, B.; Blankenberg, S. et al. (2012): How to use high-sensitivity cardiac troponins in acute cardiac care. In: European heart journal 33 (18), S. 2252–2257. DOI: 10.1093/eurheartj/ ehs154.
.jpg?width=342&height=509&name=OrtusAcademy(YELLOWGradient).jpg)




Leave Comment