Mechanical Ventilation offers a safer and more effective alternative to Manual Ventilation.
Abstract
Patients with acute life-threatening illness in the out-of-hospital setting often require assisted ventilation to ensure adequate inhalation of oxygen as well as exhalation of carbon dioxide. Ventilation is considered an essential skill in the out-of-hospital setting, but large variation exists in both how it is performed and patient outcomes. Prehospital providers may give breaths with a bag attached to a facemask, a supraglottic airway or an endotracheal tube. When performing manual ventilation with a bag, healthcare providers deliver breaths at a wide range of rates, tidal volumes and pressures, frequently deviating from recommended evidence-based practice guidelines. Such variation in care is associated with poor outcomes in patients with cardiac arrest or traumatic brain injury and may be harming other patient populations as well.
Overcoming this wide variation in manual ventilation practices would require extensive training and practice, along with vigorous quality assurance and feedback. This may be difficult to achieve without improved real-time methods of measuring ventilation rate, volume and pressure. Portable mechanical ventilators are intended to provide consistent oxygenation, as well as ventilation rate, volume and pressure. Use of these medical devices could reduce variations associated with human factors and remove a stressful and resource-heavy task, freeing up clinicians to focus on other critical assessment and treatment decisions. In addition, it would facilitate research and quality improvement efforts to expand knowledge of the impact of ventilation rates, volumes and pressures on outcomes.
Limits of Manual Ventilation in Cardiac Arrest
The potential harm caused by manual ventilation during the resuscitation of cardiac arrest patients has been well documented. Perhaps the most significant problem is simply the lack of real-time awareness of ventilation rates and volumes delivered. Aside from crude visual metrics such as chest rise and end-tidal CO2 waveform in exhaled breaths, bag-masks, whether used with facemasks, supraglottic airway devices or endotracheal tubes, provide limited guidance or feedback to the user, and no reliable method of measuring volume or pressure. Especially in the prehospital setting, where providers face distractions and competing priorities, delivering consistent breaths can be difficult—and the results of improper ventilation can be disastrous.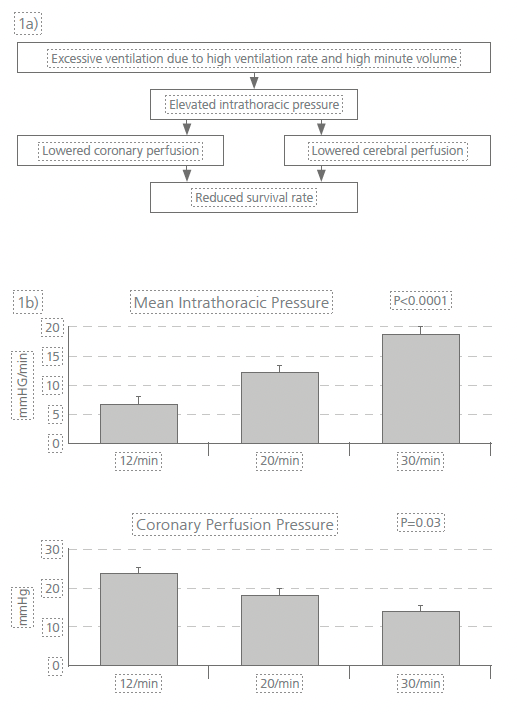 Fig 1 - a) The impacts of excessive ventilation on patients in cardiac arrest.
Fig 1 - a) The impacts of excessive ventilation on patients in cardiac arrest.
Fig 1 - b) In a study of pigs in cardiac arrest, increasing ventilation rates were associated with increased intrathoracic pressure and decreased coronary perfusion pressure. [4 Aufderheide and Lurie].
Conditions related to Manual Ventilation
Hyperventilation - Delivering breaths at too fast a rate.
Gastric Inflation - Short, pressure-driven ventilations longer than 1 second.
Barotrauma - Higher peak airway pressures,
Benefits of Mechanical Ventilation
Many countries throughout the world mandate use of prehospital mechanical ventilation for patients who require ventilation. For example, the European Union standard for medical vehicles and their equipment, EN 1789, requires mechanical ventilators for ambulances providing advanced medical care. Most ambulance services in the UK only carry supplies for manual BVM bag-valve-mask ventilation. Even those that did have mechanical ventilators, often had older models, and most were sent to hospitals during the height of the COVID-19 crisis. Therefore, manual ventilation is the paramedics only choice when a patient is experiencing respiratory failure.
Mechanical ventilators deliver ventilations at a consistent, user-derived oxygen dose, ventilation rate and tidal volume, with or without additional medications. “Controlling inflation time, flow rate, and flow waveform with a mechanical ventilator may be the best solution to control and limit peak inflation pressure for a given tidal volume,” wrote Herff and Wenzel in a comprehensive look at ventilation during resuscitation.
Pressure Limits
Mechanical ventilators with integrated pressure limits avoid excessive peak airway pressures that sometimes can occur with manual bag ventilation. [Marjanovich] Pressure is uniform with each breath, and is not impacted by the strength of the clinician or other extrinsic factors. In addition to controlling pressure, ventilators also monitor airway pressures and alert the caregivers to potential issues.
Controlled Oxygen
Many mechanical ventilators allow users to control the percent of oxygen being delivered to the patient, which can be critical for many patients on long-term ventilation.
Controlled Volume and Rate
Mechanical ventilators deliver a consistent volume with each breath, often at parameters that can be set by the clinician and adjusted to best fit the patient’s needs. Whether a patient is being ventilated with a mask or through an advanced airway device, providers can be assured that the mechanical ventilator delivers the same tidal volume each time. [L’her]
Mechanical ventilators can provide a consistent rate, eliminating one of the most persistent errors made by prehospital and other medical providers when ventilating with a bag [Nikolla]. Knowing that the ventilation rate will remain consistent allows them to focus on more adequately assessing the quality of ventilation and other patient factors.
Crew Safety and Decreased Need for Resources
Mechanical ventilation eliminates the need for a second provider during ventilation with a facemask, as the clinician can focus on maintaining a mask seal and observing the patient, without having to worry about squeezing a bag. This is still true even when an automated rate has not been set—such as during the initial, immediate response or CPR—if the mechanical ventilator allows a provider holding the mask to trigger each breath while still maintaining a two-handed seal. For EMS transport of patients who are ventilator-dependent, mechanical ventilators provide a safe and more efficient alternative to manually ventilating the patient throughout transport. Overcoming Barriers to Mechanical Ventilation
Overcoming Barriers to Mechanical Ventilation
While there are legitimate specific concerns, which are addressed below, each has to be weighed against the potential harm caused by wide variation in practice with manual ventilation, as well as the costs of continuous retraining to try to prevent that variation.
Infrequent Provider Use
Resuscitations and respiratory arrest patients requiring ventilation make up only a small percentage of emergent EMS responses. However the need for prehospital ventilation may be increasing. For example, the number of people receiving invasive ventilation at home or in skilled-nursing facilities, while unknown, is believed to have increased significantly over the last two decades. [King, Simonds] As more patients receive this treatment in the home, EMS clinicians will encounter them more often, leading to more frequent need for ventilator assistance during transport.
Cost
For many EMS systems, the purchase of any capital equipment can be a burden. However, as portable mechanical ventilators become more affordable, it is important to weigh the cost against the potential benefit, as well as the costs of other equipment. With multiple studies showing the need for frequent training to achieve optimal ventilation rates manually, there may also be a reduction in the total training time required to maintain proficiency. After recognizing the importance of consistent chest compressions, EMS systems have widely adopted mechanical CPR, despite a substantial cost to the devices. Mechanical ventilators offer many of the same benefits, with the possibility that they could be used with a wider number of patients. In addition, as reimbursement for prehospital care moves toward a value-based model, the use of mechanical ventilators to properly achieve and record certain quality metrics could be crucial.
Perceived Complexity
Although the 2007 National EMS Scope of Practice Model stated that paramedics should be knowledgeable in use of automated transport ventilators, in many systems their use appears to be limited to critical care paramedics. Whether or not an EMS clinician learned about mechanical ventilation during their initial education, it is likely that not using and frequently re-training on ventilators would lead to a lack of comfort with their use. However, ventilation with a bag-valve system is more complicated than once believed and often performed inadequately.
Studies have shown that while retraining BMV can help, it does not prevent hyperventilation or other errors, and must be conducted frequently. With the advent of safer and simpler portable ventilators, training EMS providers to use automated ventilators in specific clinical settings is quite possibly no more time consuming than training them to perform consistent, adequate and safe manual ventilations.
Weight
EMS providers encounter patients in a wide variety of settings, often requiring the movement of equipment long distances and in limited space. However, as technology and engineering progresses, many of the devices carried in the prehospital setting are becoming more compact and lighter, including monitor/defibrillators, non-invasive ventilation (CPAP) and more. Ventilators are now also available in more lightweight and rugged forms than ever before, with some weighing less than two pounds.
Conclusion
Efforts to improve resuscitation of critical patients in the out-of- hospital setting have focused on reducing variability—from mechanical CPR to “pit crew” models, the importance of standardization and adherence to guidelines has been widely accepted. Yet decades of research has indicated that wide variance continues to occur in the practice of manual ventilation of cardiac arrest victims and other critical patients encountered by EMS clinicians—variance that has been associated with negative outcomes. Mechanical ventilation offers a solution to this variance and an opportunity to provide more consistent care adhering to evidence-based guidelines now and in the future.
Contributors
The WEINMANN Emergency EMS Medical Advisory Panel is a select group of clinicians who have insight into the culture and mindset of the EMS and healthcare community. They include EMS medical directors and researchers who are among leading experts in resuscitation and prehospital medicine. The group contributed expertise, editorial advice and review for this paper. Final responsibility for authorship and the content of the report was retained by WEINMANN Emergency.
Jan-Thorsten Gräsner, MD, FERC, Andrew McCoy, MD, MS, Graham Nichol, MD, MPH, FRCP(C), FACP, FAHA, Scott Youngquist, MD, MSc.
References
Marjanovic N, Le Floch S, Jaffrelot M, L’Her E. Evaluation of manual and automatic manually-triggered ventilation performance and ergonomics using a simulation model. Respiratory care. 2014;59(5);735-742.
King AC. Long-term home mechanical ventilation in the United States. Respiratory care. 2012;57(6):921-32.
Want to learn more?
Visit The Ortus Group website to see our range of WEINMANN Mechanical Ventilators:
https://www.theortusgroup.com/medical/medical-ventilation/
.jpg?width=342&height=509&name=OrtusAcademy(YELLOWGradient).jpg)




Leave Comment